Introduction: A New Weapon Against Invisible Enemies
Imagine a world where the antibiotics that once saved millions now fail against ruthless bacterial invaders in our lungs. Multidrug-resistant (MDR) bacterial pneumonia isn't just a medical headline—it's a ticking time bomb in hospitals worldwide, claiming lives and straining healthcare systems. The antibiotic resistance crisis has escalated from a looming threat to a daily reality. But recent breakthroughs are reigniting hope. A groundbreaking study from researchers at the Icahn School of Medicine at Mount Sinai, published in Nature, introduces an mRNA-based therapy that delivers antimicrobial peptides (AMPs) directly to the lungs. By transforming AMPs into 'peptibodies' packaged in anti-inflammatory lipid nanoparticles, this approach not only combats resistant bacteria but also tames the inflammation that often worsens the damage. This isn't just another tweak to existing drugs; it's a paradigm shift that could redefine how we fight respiratory infections.
The Crisis of Antibiotic Resistance and the Promise of AMPs
The global antibiotic resistance crisis poses a severe threat to public health. According to the World Health Organization, antimicrobial resistance could cause 10 million deaths annually by 2050 if unchecked. In the lungs, MDR pathogens like methicillin-resistant Staphylococcus aureus (MRSA) and carbapenem-resistant Pseudomonas aeruginosa thrive, turning routine pneumonias into lethal battles. Traditional antibiotics are losing ground as bacteria evolve faster than we can develop new ones.
Enter antimicrobial peptides—nature's ancient antibiotics produced by our immune systems and countless organisms. AMPs, such as defensins and cathelicidins, punch holes in bacterial membranes, offering broad-spectrum killing power without the rapid resistance buildup seen in conventional drugs. Yet they face a critical challenge: delivery. AMPs degrade quickly in the bloodstream, struggle to reach infection sites in sufficient quantities, and trigger excessive inflammation, which can exacerbate lung damage in pneumonia patients. Direct administration often requires high doses, leading to toxicity and poor bioavailability. This is where innovation steps in, turning theoretical promise into practical therapy.
Breaking New Ground: Peptibodies and mRNA Delivery
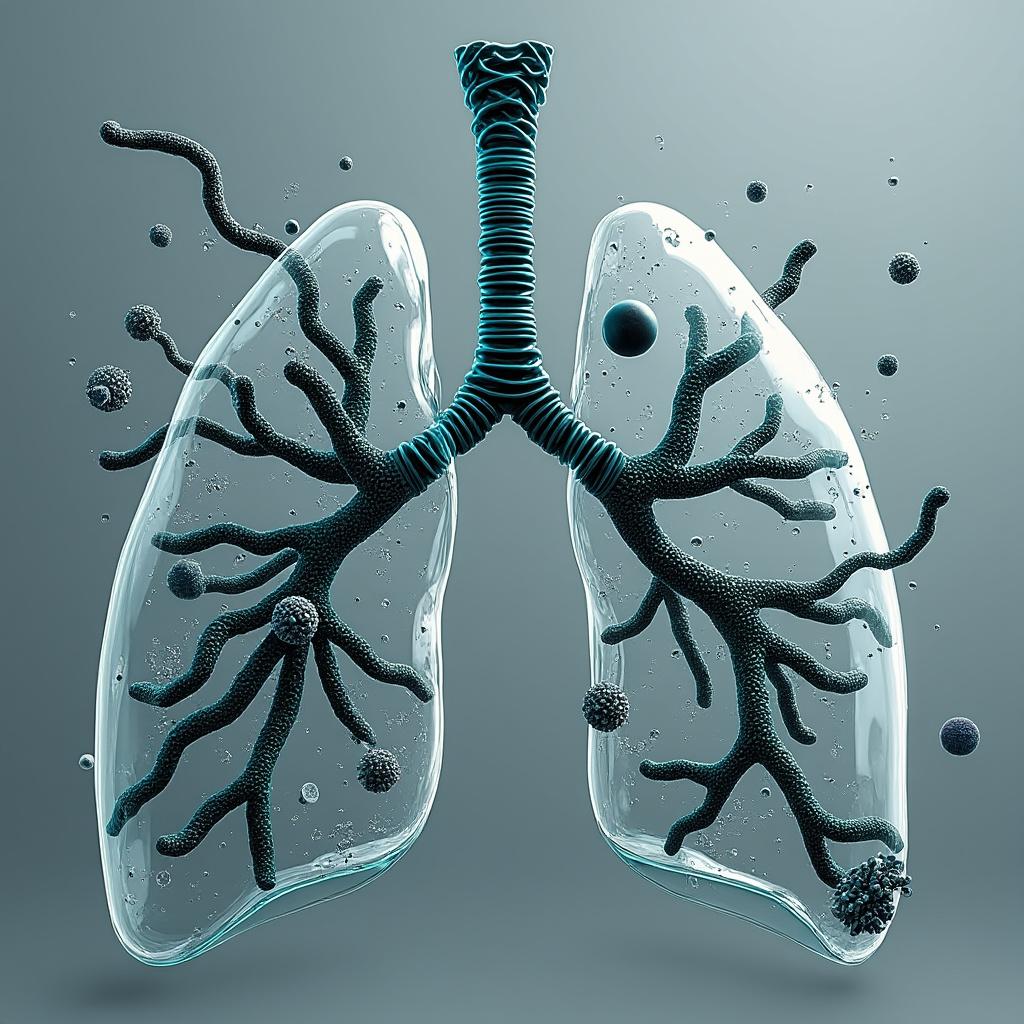
The Mount Sinai team's ingenuity lies in repurposing mRNA technology—famous for COVID-19 vaccines—to encode AMPs as 'peptibodies.' These are fusion proteins where the antimicrobial peptide is linked to an antibody fragment, enhancing stability and targeting. Instead of injecting fragile AMPs, the therapy delivers mRNA instructions via lipid nanoparticles (LNPs). Once inhaled or administered to the lungs, lung cells act as on-site factories, producing the peptibodies locally and precisely where needed.
What sets this apart is the nanoparticle formulation. The researchers incorporated anti-inflammatory lipids, such as those mimicking resolvins or specialized pro-resolving mediators, into the LNPs. This dual-action design doesn't just kill bacteria; it modulates the inflammatory storm that accompanies severe pneumonia. In preclinical mouse models of MDR pneumonia, the therapy achieved up to 90% bacterial clearance, far surpassing traditional AMP delivery or even some last-resort antibiotics. The mRNA ensures sustained production—peptibodies lingered in lung tissue for days, maintaining therapeutic levels without repeated dosing.
This convergence of mRNA and AMP research is elegant. mRNA's transient expression avoids genomic integration risks, and the localized production bypasses systemic side effects. The study, detailed in Nature (doi:10.1038/s41587-025-02928-x), used advanced imaging to confirm peptibody accumulation in alveolar macrophages, the lung's frontline defenders, highlighting the precision of this delivery system.
Expert Insights and Broader Implications
Experts are enthusiastic about this development. The anti-inflammatory lipids are a standout feature; they not only reduce cytokine storms but also promote resolution of inflammation, potentially shortening recovery times and preventing long-term lung scarring.
This work builds on mRNA's post-COVID momentum. Platforms like those from Moderna and BioNTech, once virus-focused, now extend to bacterial threats, aligning with precision medicine trends. Imagine tailoring peptibodies to specific MDR strains via rapid mRNA synthesis—a customizable arsenal against evolving pathogens. Beyond lungs, similar approaches could target MDR urinary tract infections or wound sepsis.
The implications ripple outward. For FDA approval, this could fast-track AMPs previously shelved due to delivery issues, slashing development timelines. Economically, it addresses the billions in annual costs from MDR infections. Ethically, it democratizes access to advanced therapies, especially in low-resource settings where pneumonia kills millions yearly. This represents a blueprint for combination therapies: antimicrobial action fused with immunomodulation, tackling resistance holistically.
Conclusion: Toward a Resistant-Free Future
This mRNA-peptibody therapy isn't a silver bullet, but it's a powerful salvo in the war on antibiotic resistance. By enabling lungs to produce their own defenses while soothing inflammation, it addresses the core flaws of AMPs and the desperation of MDR pneumonia. Looking ahead, clinical trials will be crucial to translate these preclinical wins into human success, but the foundation is solid. If scaled, this could save countless lives, proving that innovation born from crisis—like the COVID era—holds the key to tomorrow's cures. The resistance era may be upon us, but with tools like this, we're not defenseless.
Brief Summary
This article explores a pioneering mRNA therapy that delivers antimicrobial peptibodies to the lungs via anti-inflammatory nanoparticles, effectively treating multidrug-resistant bacterial pneumonia. Drawing on the latest research from Mount Sinai, it highlights how this approach overcomes traditional delivery barriers and integrates inflammation control for superior outcomes. The innovation promises to expand mRNA's role beyond vaccines, offering hope in the fight against global antibiotic resistance.